-
Radiation Therapy
-
Radiation Therapy
back
-
Categories
-
Categories
back
-
Detectors
-
Detector Arrays
-
Water Phantoms
-
QA Phantoms
-
Electrometers
-
Software Solutions
-
Categories
- Machine QA
-
Treatment Modalities
-
Treatment Modalities
back
- FLASH Therapy
- IMRT/VMAT
- SRS/SBRT/SRT
- MR-Guided Radiotherapy
- Proton/Particle Therapy
- Brachytherapy
-
Treatment Modalities
- Patient QA
-
Treatment Machines
-
Treatment Machines
back
- C-arm Linacs
- Bore-type Linacs
- SRS Linacs
- GammaKnife
- CyberKnife
- ZAP-X
- TomoTherapy/RadiXact
- Proton Therapy Systems
- MR-Linacs
-
Treatment Machines
-
Radiation Therapy
-
Diagnostic Imaging
-
Diagnostic Imaging
back
- Categories
-
Imaging Quality Control
-
Imaging Quality Control
back
- NORMI RAD/FLU
- NORMI 3D
- X-Check DSA
- NORMI 13
- NORMI MAM digital
-
Imaging Quality Control
-
Patient Dosimetry
-
Patient Dosimetry
back
- DIAMENTOR Systems
- DIAMENTOR C-RS
- DIAMENTOR RS-KDK
-
Patient Dosimetry
-
Acceptance Testing
-
Acceptance Testing
back
- NOMEX Dosemeter
- NOMEX Multimeter
-
Acceptance Testing
-
Treatment Modalities
-
Treatment Modalities
back
- Radiography and Fluoroscopy
- Mammography
- Computed Tomography
- Dental Radiography
- X-Ray Radiation Therapy
- Cone-Beam CT
-
Treatment Modalities
-
Diagnostic Imaging
-
Radiation Monitoring
-
Radiation Monitoring
back
- Electrometers
- Ionization Chambers
- Survey Meters
- Personal Dosemeters
-
Radiation Monitoring
- OEM
- Metrology
Product Highlights
BEAMSCAN
Water Phantoms
UNICHECK
Web-based Daily QA
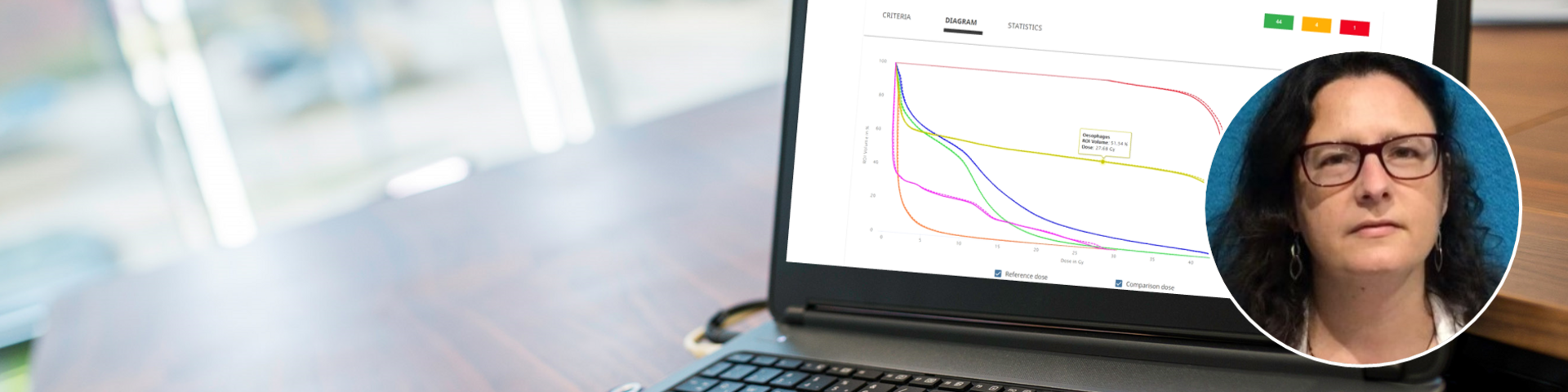
VERIQA
Patient QA Platform
RUBY
Modular QA Phantoms
BEAMSCAN MR
Water Phantom for MRgRT
OCTAVIUS 4D / 4D MR
QA Phantom
Electron Density Phantom
Classical Shape Phantom
Track-it
QA Data Management Platform
flashDiamond
Detector
UNIDOS Tango & Romeo
Reference Class Electrometers
Product Highlights